(Originally published to Sam’s Caring Bridge site on 5.15.18. To read all previous entries from Sam’s NICU journey, visit his Caring Bridge site: https://www.caringbridge.org/visit/samueldwenger)
Samuel was born via cesarian at 10:20pm on Monday, May 7th. At Southview where Samuel was born he was checked out and treated by two nurses. He received breathing tubes in his nose and was prepped for an ambulance ride. They added little heart-shaped stickers that I later learned were there to attach body temperature probes to monitor him. Dayton Children’s provided the ambulance service, and when they arrived at Southview they wheeled Samuel into the recovery room that Liz, her mom and I were in for one last look before taking him away to Kettering for his stay in the NICU. He left Southview at around 1am. Liz would stay behind for two nights recovering from her procedure. I went to Kettering NICU after Sam and was in the room for the nurses and doctor’s initial assessments and treatments. Dr. Hill and nurse Megan were primary care with other respiratory therapists and nurses assisting (I did not think to get all of their names at the time). I watched as they put a feeding tube down his mouth, gave a surfactant treatment to help open up his lungs (that are not fully developed in a 29-week old) and hooked up a CPAP machine to help him get more oxygen pumped into his lungs. Every 30 minutes they drew blood from his foot to check his glucose levels (his levels were very low). They had an IV in his arm to provide fluids and nutrients that he needed, but after a couple of hours the doctor came back in and said that they needed to put in an unbilical cord IV to give him a higher concentration of nutrients to help him stabilize. They had to take me out of the room for about an hour while they performed this procedure, which they completed successfully and allowed for him to stabilize more quickly.
I think I slept for about 45 minutes that night during a brief lull between nurses coming into the room and while the monitors he was hooked up to either stopped beeping or I get used to them enough to not let them bother me.
Tuesday was about learning everything that I could about Samuel’s health, asking as many questions as I could and processing as much information as possible. This was in part because that’s how I am, and in part because Liz was still at Southview and I felt it was important to give her all of the information that I could get to keep her calm and let her know what was going on and what all of the information meant. Sam is hooked up to several devices that constantly monitor how he’s doing and administer medication. 2-3 tubes provide lipids, caffeine and antibiotics. When each of these machines is pumping you hear a little ‘tick’ sound of the pump working. The CPAP machine always has a ‘hiss’ of the oxygen running into the tube assisting his breathing, while a second tube ‘bubbles’ in a cup of liquid to help keep humidity in the air. This bubbling is constant, except for when Sam opens his mouth and doesn’t use it (which he’s not supposed to do and always scares us a little that he isn’t breathing at all).
This is probably the worst of the monitors because of how it looks on him. It is large and goes into his nose so you can’t see his face, and it mounts onto a cap on his head and straps around it. Liz likes to call the CPAP hat his “fighter pilot hat” because with the white hat and black strap it looks like something from Top Gun.

The bed shows his body temperature (should be around 36.5 Celsius) as well as the temperature of the bed, which changes based on how Sam’s temperature changes. The bed also has humidity controls, which at the beginning were set to 60%. Liz calls his incubator bed his “spaceship” because of how automated the controls are and how it can move up, down, the lid comes off, and the nifty touch screen controls it has. Lastly, the things we love and hate the most – the monitors that track his key vitals. They keep track of his heart rate (green), respiratory rate (yellow), oxygen levels (blue), and blood pressure (white). We love these monitors because when he’s sleeping and peaceful and the numbers look good we can tell by looking at them everything is ok and he’s doing well. We hate these monitors because the second they beep, we fear the worst. This is maybe one of the hardest things for me each day is sitting in the room, trying to clear my mind, pray, or just relax, and you hear a beep on a monitor that makes you fear the worst. In a week there hasn’t been anything that he’s had that’s been life-threatening (praise the Lord) but I believe it’s the first feeling of “parent” in me that comes out when these alarms go off.
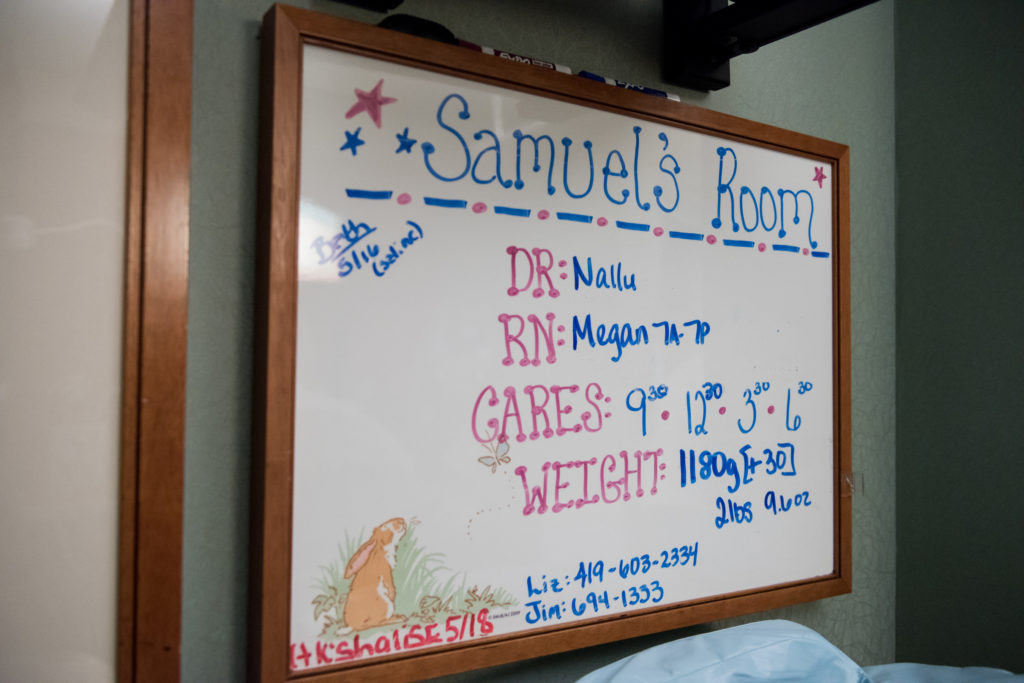
Every day at around 10am there are “rounds”. These are very nice to be there for, as the doctor, nurses, respiratory therapist, pharmacist, occupational therapist and anyone else who can help with any of the children goes room by room to discuss the status of each baby and the treatment that baby will receive for the day. It’s a great time to ask any questions, talk to anyone on Sam’s care, or just see how great the teamwork is between everyone on the staff to take care of every child in the NICU.

Wednesday was a much more difficult day to be with Samuel. They day started off great. I was able to hold him skin to skin for the first time. I was nervous about holding him as he is so fragile and I am so inexperienced with babies, but once I got to touch him I had no worries and he slept on my chest for nearly two hours before it was time to put him back for his care. His jaundice level was high (8.6) so he had to undergo Bilirubin light therapy, which is a blue light they shine on his body to help the red blood cells in the body. He has to wear a protective, padded shield over his eyes while this light is on, and because his levels were so high the light had to be on 24 hours a day for three days. Having this light on also means that skin time is limited. Liz was discharged on Wednesday night and came to the hospital about 6:30pm. She was still in a lot of pain and her blood pressure was not yet stabilized with the medication, but she came in time to hold Sam for the first time. We shared a lot of tears and love in the hour she held him. We then tried to get comfortable for both of us to stay the night in the room…which wasn’t the best idea. Our room in the NICU has a reclining chair, a rocking chair and a rolling chair. Sleeping in the recliner is doable, but the other two offer less than desirable comfort. We took turns in the recliner as neither of us could sleep, Liz from her continued pain and me from never being able to get comfortable.
